Mohs Surgery
What is Mohs Surgery?
Mohs surgery is the gold-standard technique for the removal of skin cancers including basal cell cancers (BCC) and squamous cell cancers (SCC). It was developed in the 1930s by Dr. Frederic Mohs in the USA and brought to Australia in the 1980s. It is the world's most effective and precise technique for removing skin cancer.
Mohs Surgery offers the highest cure rates (up to 99%) and the smallest scars.
The goal of Mohs surgery is to remove the skin cancer completely, while preserving as much healthy tissue as possible. Many skin cancers are like icebergs with invisible roots extending either along the surface of the skin or deeper into the tissue. This highly specialised technique allow the specialist to carefully track the roots of the cancer under the microscope to ensure they have all been removed prior to reconstruction. This ensures that clear margins are obtained before the reconstruction is performed and avoids the need for reexcision due to close or incomplete margins. Mohs microgrpahic surgery allows precise examination of 100% of the skin cancer margins, compared to only approximately 1% of the margins typically assessed with standard surgery.

When is MOHS recommended?
-
Mohs surgery is the best treatment for skin cancers:
-
Most facial non-melanoma skin cancers
-
Cosmetically and functionally important sites (see below)
-
Recurrent, residual or incompletely excised non-melanoma skin cancers - especially facial.
-
Poorly-defined clinical margins
-
Aggressive subtypes including infiltrating, micronodular, sclerosing, morphoeic and mixed morphology e.g. superficial and nodular, basosquamous carcinoma and rare skin tumours
-
Perineural invasion on histology
-
Large, aggressive or rapidly growing BCCs or SCCs.








Who can perform MOHS SURGERY?
Fellowship-trained Mohs specialists are qualified dermatologists who have undergone additional fellowship training in Mohs surgery. This training includes examination of skin cancers under the microscope, tracking and excising the roots of skin cancers and repairing the area where the cancer was surgically removed with either a line scar, skin graft or skin flap.
RECONSTRUCTION POST MOHS SURGERY
Dr O'Sullivan offers same-day reconstruction following excision of the cancer. This can be done under her care, or under the care of a trusted, specialist plastic and reconstructive surgeon or oculoplastic surgeon, on the same day in the same hospital. In rare or complex cases, a reconstruction can offered at another
hospital and/or another day if required.
What does the procedure involve?
-
The surgery is typically conducted in a day surgery unit.
-
Medication such as diazepam can be used to reduce anxiety prior to surgery if required.
-
Dr. O'Sullivan carefully marks the area where the skin cancer is and numbs the area with a local anaesthetic.
-
Targeted special injections known as nerve blocks can be used to provide long-lasting pain relief and anaesthesia to help reduce the need for extra injections.
-
The visible portion of the skin cancer along with a thin margin of normal tissue is removed using a scalpel.
-
A temporary bandage is placed on your wound.
-
The cancer is carefully orientated using special ink and a bespoke map is made of your cancer. The tissue is then frozen and processed in an on-site laboratory.
-
Microscope slides are made with the removed skin cancer tissue. This process can take 30-90 minutes.
-
Dr. O'Sullivan then checks the microscope slides for any remaining cancer cells along the edges of the tissue. 100% of the margins are meticulously assessed under the microscope including the edges and the base of the cancer.
-
Should any roots remain, the process is repeated with additional layers (or stages) taken until all the cancer is cleared. For most people the procedure takes just a few hours but there is a very small chance that it could take all day.
-
After the cancer has been completely removed, your wound can be left to heal on its own or repaired; depending on the extent of the procedure.
Types of repairs/reconstructions include:
-
Left to heal naturally (by secondary intention)
-
Side-to-side closure – using stitches to close the wound
-
Skin graft – using skin from another part of the body to cover the wound
-
Skin flap – moving skin from an adjacent area to cover the wound

WHAT DOES THE CANCER LOOK LIKE UNDER A MICROSCOPE?
There are many subtypes of basal cell and squamoius cell cancer, as well as rarer tumours. They all look different under the microscope, here are some examples:

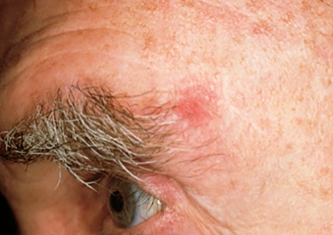
BASAL CELL CARCINOMA

BASAL CELL CARCINOMA

BASAL CELL CARCINOMA
SQUAMOUS CELL CARCINOMA
How does Mohs surgery differ to standard surgery?
Standard surgery involves removing the visible cancer and a small margin of surrounding healthy tissue all at once. It relies on Dr. O'Sullivan being able to see the extent of the cancer to determine a safety margin to cure the cancer. However, basal and squamous cell cancers often have invisible roots that cannot be seen by the naked eye.
Standard surgery may estimate a larger safety margin than is required to cure the cancer, resulting in a larger scar with too much healthy tissue being removed. Conversely, too little tissue may be removed, leaving roots in place and increasing the chance of the cancer recurring, requiring further, more complex surgery.
Mohs surgery maximises the chance of complete cure of the cancer and minimises the need for more difficult revision surgery should the cancer return.
The main difference with Mohs is the length of time the procedure can take, as each layer must be individually analysed. This takes longer than traditional cancer excisions. However, in most cases it is worth spending the extra time to be certain the entire cancer has been removed. It allows verification that all cancer cells have been removed on the day. Mohs surgery is associated with higher costs, due to the expertise required, complexity and time-consuming nature of the procedure.
When should I have surgery?
It is important to get any skin cancer treated at the earliest possible time to help minimise the size of the scar and the complexity of the surgery. The longer a tumour is left, the greater the risk that the cancer can spread,necessitating wider, deeper, more complex surgery.
What would happen if I left my cancer untreated?
If untreated, the cancer will continue to grow beneath the surface of the skin. It may grow into nerves, blood vessels or lymphatics, or cause pain and bleeding. It may break the surface of the skin and form an ulcer.
Basal cell cancers are also known as “rodent ulcers” because if untreated they become larger and may develop deep roots, eating away at skin, nerves and underlying tissues (including cartilage, bone and eye tissue), requiring more complex surgery to remove and reconstruct the wound left behind. It is extremely rare for basal cell cancers to spread to the rest of the body.
Squamous cell cancers, however, can spread to the body and may be fatal if left untreated. Recent evidence shows that there are motre deaths from squamous cell cancers than melanoma globally.
Do I still need surgery if my biopsy area appears to have healed?
Yes, most skin cancers have invisible roots beneath the surface of the skin which are not seen by the naked eye. In most cases, your biopsy was performed to provide a diagnosis, but not to treat it.
The surface of the wound may appear to have healed but, beneath the surface roots remain. By the time the skin cancer grows back from its roots and becomes obvious on the surface, deeper invasion may have occurred.
Will there be a scar?
A scar after surgery is a certainty - there is no such thing as invisible mending. Mohs surgery allows for the smallest scars as only unhealthy tissue is removed. The size and shape of the scar will only be determined after the cancer and all its roots have been removed. We endeavour to hide the scar within the natural creases of the face, however sometimes this is not possible due to the complexity or size of the cancer. I work closely with some of the best plastic surgeons optimise aesthetic and functional outcomes, especially in difficult areas.
All scars take 12-18 months to finally settle and mature, and you will be provided with scar-care advice.
Can I just use a skin cancer cream or have the skin cancer frozen (liquid nitrogen cryotherapy)?
Every skin cancer and individual are different. Some surface cancers can be treated with skin cancer creams, photodynamic therapy or liquid nitrogen cryotherapy, however this is only suitable for certain surface skin cancers, and suitability will be determined the specialist after close examination with a dermatoscope and a slide review of the pathology and report. The cure rates for these non-surgical techniques are lower than with surgery and the recurrence rate is higher. Sometimes, inappropriate treatment of a skin cancer with a cream, light or freezing treatment can polish the surface of the skin and delay detection of a more serious cancer. The biopsy does not always tell the whole story and this is why a specialist review of your report and targeted examination is essential to provide you with the best management options for your cancer.
What if my cancer has previously been treated and has come back?
Mohs surgery is the gold standard for recurrent cancers anywhere on the body, as it allows examination of 100% of the margin and provides the highest cure rate. In person assessment and histological review, coupled with precise surgery leads to the best outcomes.
Where can I get more information?
Please visit The American College of Dermatologists’ website.
American College of Mohs Surgery: https://www.mohscollege.org
Mohs Surgery: https://www.dermcoll.edu.au/atoz/mohs-surgery/
Find a Mohs Specialist: https://www.dermcoll.edu.au/find-a-derm/find-a-mohs-specialist/
References
-
Etzkorn JR, Alam M. What Is Mohs surgery?. JAMA Dermatol [Internet]. 2020 May 6 [cited 2022 Aug 31];156(6):716. Available from: https://jamanetwork.com/journals/jamadermatology/fullarticle/2764796 DOI:10.1001/jamadermatol.2020.0039
-
Mayo Clinic. Mohs surgery [Internet]. Scottsdale AZ: Mayo Clinic; 2022 [updated 2022 Aug 23; cited 2022 Aug 31]. Available from: https://www.mayoclinic.org/tests-procedures/mohs-surgery/about/pac-20385222
-
National Cancer Institute. Mohs surgery. [Image on Internet]. 2010 [updated 2010; cited 2022 Aug 31]. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/mohs-surgery
-
American College of Mohs Surgery. Post-operative care [Internet]. Milwaukee WI: American College of Mohs Surgery; published date unknown [updated date unknown; cited 2022 Aug 31]. Available from: https://www.mohscollege.org/for-patients/about-mohs-surgery/post-operative-care
-
Yiasemides E, Sheridan A. Mohs surgery [Internet]. St Leonards NSW: The Australian College of Dermatologists; 2019 [updated 2019; cited 2022 Aug 31]. Available from: https://www.dermcoll.edu.au/atoz/mohs-surgery/



